In 1982 my professional (ICAS) practice career took me to The Big Apple a few months before the incorporation of ACAUS. I went to work with Roger Musson, the first ACAUS President following on from founder Angus McDowell. I lived and worked in the USA until 1985 having taken over from Roger as the Deloitte Haskins & Sells UK/US Liaison Partner in the USA.
I guess my most memorable claim to ACAUS fame, as Ian Wise reports in his book ‘ACAUS The First 40 Years’, was finding haggis for 150 diners at the very first formal ACAUS dinner in 1983 at Windows on the World atop the late Twin Towers….. or, as Roger Musson used to refer to it from our offices on Floor 100, “the office canteen”! Even in their natural habitat of the wilds of the Scottish Highlands haggis do not tend to fly to such altitudes.
In the early ‘Noughties’, after 30 years I decided to leave the Firm (now PwC) and try ‘other things’ while I still had all my faculties! The next 4 years saw a number of Board appointments, including at Birmingham Specialist Children’s Hospital (BCH) which saw my wife Alexis and I ‘take a holiday’ to Malawi to consider a project to which some consultant paediatricians at BCH wanted Board permission to contribute their time and skills.
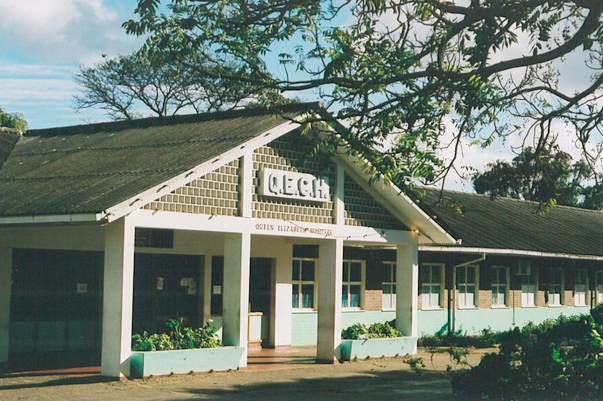
The project base was within Malawi’s largest State hospital The Queen Elizabeth Central Hospital, Blantyre (QECH).
Monday 30 July 2007 at 11.00 am was a life changing moment for us both as we were confronted with the stark realities of healthcare in one of the very poorest nations in the world. The sights, sounds and smells were overpowering and the facts and figures were shocking.
We returned home from Africa dazed but determined to try to do something to help the small number of expat British and Dutch doctors who were establishing a paediatric healthcare offering where there was none for the 50% of the population who were children ie under the age of 18 years. By comparison, the under 18s make up about 25% of the UK, Europe or USA populations. Life expectancy in Malawi is roughly 20 years less than those areas.
The ‘Brain Drain’ from Malawi had resulted in there being no Malawian paediatricians practising in their own nation. Treating children medically as if they were adults contributed to the shocking mortality rates.
The project focused on not just building effectively a Children’s Hospital within the nation’s largest State Hospital but significantly impacting and delivering the curriculum at the nearby Malawi School of Medicine as regards paediatrics. The concept assumption was that if Malawians are trained to world standards in their own nation then they will be more likely to remain in Malawi and, after qualifying, become the sustainable future of paediatric healthcare in their own nation. The assumption has proved to be sound.

So, on return home to the UK and not being medical, my wife and I decided to set up a UK registered charity, Friends of Sick Children in Malawi (FOSCiM), and try to raise money to support the aims of the medical team pioneering in Malawi.
If anyone had told this ICAS member that on leaving PwC in 2003 I would soon after find myself pre-occupied with paediatric healthcare in one of the poorest nations of the world I would have called them crazy but here we are – 14 years on and still doing what we can.
The following table offers one stark look at just part of the challenges, but also a measure of the progress that has been made and gives a sense of the remaining challenges.
Child Mortality (per 1,000 live births)
| Malawi | UK | USA | ||
|---|---|---|---|---|
| 2000 | 2020 | Current | ||
| Neo nates < 1 month old | 39 | 20 | 2.8 | 3.7 |
| Infants < 1yrs | 100 | 31 | 3.7 | 5.6 |
| Child < 5yrs | 173 | 42 | 4.3 | 6.5 |
| Malawi child in-patient mortality | 1 in 5 | 1 in 20 | 1 in 100 | |
N.B. Paediatrics covers all children up to the age of 18 years not just the under 5s. Maternal mortality has also come within the project’s orbit. Similar positive progress has been made across both those groups.
None of us take any money from the charity so in 2020 for example 99.2p of every £1 received by FOSCiM from donors was applied for frontline needs in Malawi and we are obsessive about the stewardship of donor money. The latter may have something to do with my personal and professional roots!
I soon discovered that applying to philanthropic donors the same relationship management approach that I used for clients when in the profession was greeted positively and with surprise. Some donors in NYC said to me that they are increasingly fed up with the big well known charities; they never have contact with the people behind the charities and regard their fundraising as akin to ‘rape and pillage’! They take your money then you don’t hear from them again until they want more.
Education and Innovation are essentials at the heart of the progress that has been made.
This means educating Malawians to World standards in paediatric healthcare.
Innovation includes developing affordable tools in the face of the often unreachable costs of medical equipment from the wider world.In 2013 the team in Malawi, collaborating with Rice University of Houston Texas, developed an affordable CPAP* machine that won first prize in the inaugural Glaxo Smith Kline – Save the Children Global Award for Innovation in Child Healthcare.
*Continuous Positive Airway Pressure

To understand how INNOVATION is so important in this context please watch this 15 minute TED MED talk: How a neo-natal health innovator saves lives in Malawi The Malawian speaker, a friend and colleague, is now the most senior paediatrician in Malawi and recently became The Director of Health for Malawi………and she gives a moving but also powerful short presentation.

In a lighter moment for the camera, my wife Alexis and I with two of the amazing Malawi team at The Queen Elizabeth Central Hospital Paediatrics Department.
Both ladies were funded by our donors through, in one case a four year BSc.(Hons) Degree in Child Health at the University of Mzuzu and in the other case a similar qualification through The Kamuzu College of Nursing.
Much has been achieved by colleagues in Malawi but many challenges remain, not least to continue to bring the shockingly high infant, child and maternal mortality rates nearer to those that we experience in the so-called First World.
FUNDS are needed for many things but primarily for:
- Educating Malawians in their own nation to world standards in paediatrics; doctors, nurses and clinical officers – the costs of which are a fraction of the equivalent in the UK, Europe or the USA;
- Innovating to develop and make more medical equipment and ‘tools’ affordable and relevant to under-developed and under-resourced settings. Developing the people takes us so far but the people need the tools to successfully apply their skills;
- Creating new facilities such as the recently created High Dependency Unit for Children (HDU) and for upgrading existing facilities such as the Children’s Accident & Emergency building to meet the increasing demand because of the success of this project.
Donors have ensured the funding of the HDU.
The funding for upgrading the indispensable Children’s Accident & Emergency unit currently has a funding gap of roughly £130,000 / $180,000. I say ‘roughly’ because if an application for relief from VAT is approved then the gap may reduce. Whatever the outcome there will still be a gap to fill.
Our current PAEDIATRIC healthcare offerings developed at our base hospital are as follows and all have wards or similar appropriate facilities:
- Accident & Emergency unit – point of entry for almost 100,000 child patients in a year. 25% of these children are admitted as in-patients.
- High Dependency Unit
- Medical Bay for chronically ill and neurological problems
- Special Care for the very ill
- Oncology
- Orthopaedic
- Malnutrition treatment
- Clinics for babies born outside of the hospital
- Neo-natal with high dependency facility
- Kangaroo Care for premature babies
- One Stop Centre for victims of abuse – children, girls and women
- Specialist outpatient clinics for HIV care, heart disease, neurological problems, sickle cell disease, TB, renal disease, diabetes, and general paediatrics
Also,
- Classroom and teacher for the child patients (and their siblings). For some this can be their first taste of schooling and they absorb it like sponges.
Malawians who have come through this project are now practising in the capital city and elsewhere in Malawi thus spreading the paediatric coverage nationwide.
There are many needs to satisfy to allow each of these offerings to function in such a resource poor environment where augmenting what the State provides is often a necessity rather than a luxury, and we are fortunate to have a number of generous and loyal supporters who help us as much as they can.
More supporters are always needed and sought.
If you would like to help please contact me on gordon@friendsofsickchildreninmalawi.org

Professor Liz Molyneux, one of the architects of sustainable paediatrics in Malawi, on duty in the Children’s Accident & Emergency Unit, the entry point for all sick children presenting at the hospital.
In Malawi the hospital entrance is the entry point for primary, secondary and often tertiary healthcare.



 IN CONCLUSION, I feel that my background as a chartered accountant has served me well with FOSCiM in a number of respects. In a situation where there are never enough medical human and other related resources, I like to think that amongst other things I have been able to establish and develop relationships with donors in various parts of the world including Malawi, raised funds for a number of important aspects of the work in Malawi, brought some non-medical order to the departmental back office in Malawi, and generally raised the profile in the World of what colleagues are doing in Malawi.
IN CONCLUSION, I feel that my background as a chartered accountant has served me well with FOSCiM in a number of respects. In a situation where there are never enough medical human and other related resources, I like to think that amongst other things I have been able to establish and develop relationships with donors in various parts of the world including Malawi, raised funds for a number of important aspects of the work in Malawi, brought some non-medical order to the departmental back office in Malawi, and generally raised the profile in the World of what colleagues are doing in Malawi.
On leaving PwC I never for one moment contemplated how I would spend the last 14 years and the foreseeable future as regards what we try to do for Malawi but despite all the many frustrations of ‘doing business in Africa’, I am grateful for that moment at 11.00 am on Monday 30 July 2007.
If you would like to help in any way please do not hesitate to contact me gordon@friendsofsickchildreninmalawi.org
